In this article, CVS Health, UnitedHealth Group, and Cigna have filed a lawsuit against the Federal Trade Commission, alleging that the agency’s case regarding drug supply chain middlemen and high insulin prices in the U.S. is unconstitutional. The complaint was lodged in the U.S. District Court for the Eastern District of Missouri, marking the latest development in a contentious legal battle between the three largest pharmacy benefit managers (PBMs) in the U.S. and the FTC.
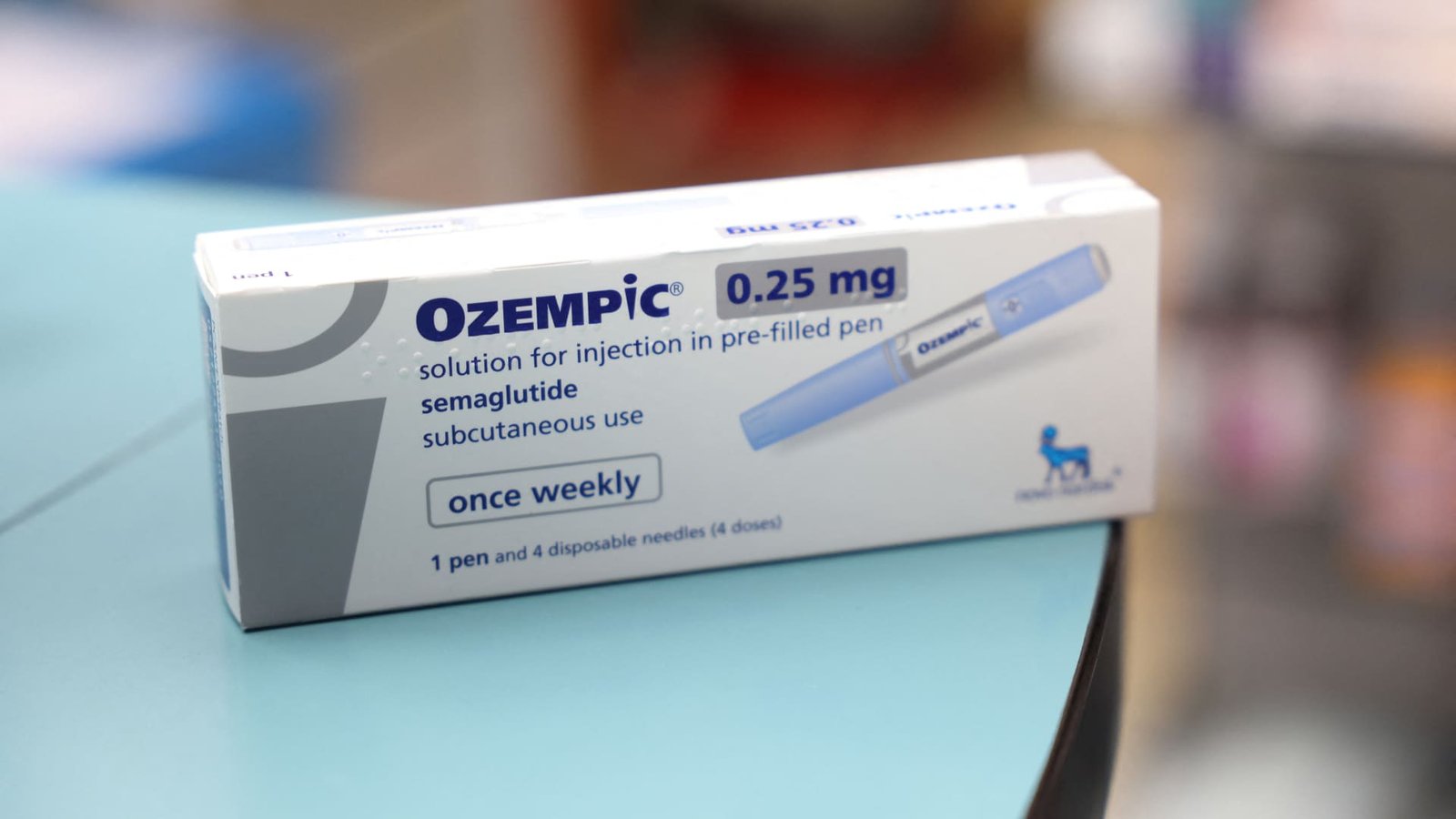
The FTC had previously sued CVS’s Caremark, Cigna’s Express Scripts, and UnitedHealth’s Optum Rx in September, accusing these PBMs and other drug middlemen of utilizing a “perverse” rebate system to increase their profits while driving up insulin costs for Americans. The FTC’s administrative process involves a proceeding before an administrative judge who would hear the case, followed by a vote from FTC commissioners on that opinion.
The complaint filed on Tuesday argues that the FTC’s process violates the companies’ due process rights under the Fifth Amendment. The companies also contend that the FTC’s claims involve private rights that should be adjudicated in federal court rather than the agency’s in-house administrative court. They criticize the process as “fundamentally unfair,” highlighting that commissioners and an administrative law judge are “unconstitutionally insulated from removal by the President and thus are insulated from democratic accountability.”
The companies assert that the attempt to reshape the industry through law enforcement would not be acceptable in a U.S. district court. In response, FTC spokesperson Douglas Farrar stated that it is a trend for corporate giants to challenge the constitutionality of a 110-year-old federal agency to divert attention from alleged harmful business practices, particularly in the case of PBMs affecting patients by imposing high costs for life-saving medication.
PBMs play a crucial role in the U.S. drug supply chain by negotiating rebates with drug manufacturers for health plans, reimbursing pharmacies for prescriptions, and determining the list of medications covered by insurance. The lawsuit follows a previous demand by CVS, UnitedHealth Group, and Cigna for FTC Chair Lina Khan and two other commissioners to recuse themselves from the agency’s in-house suit due to perceived bias against PBMs in public statements. Caremark, Express Scripts, and Optum Rx, all linked to health insurers, collectively manage around 80% of the nation’s prescriptions, according to the FTC.